There's no place like home for your recovery
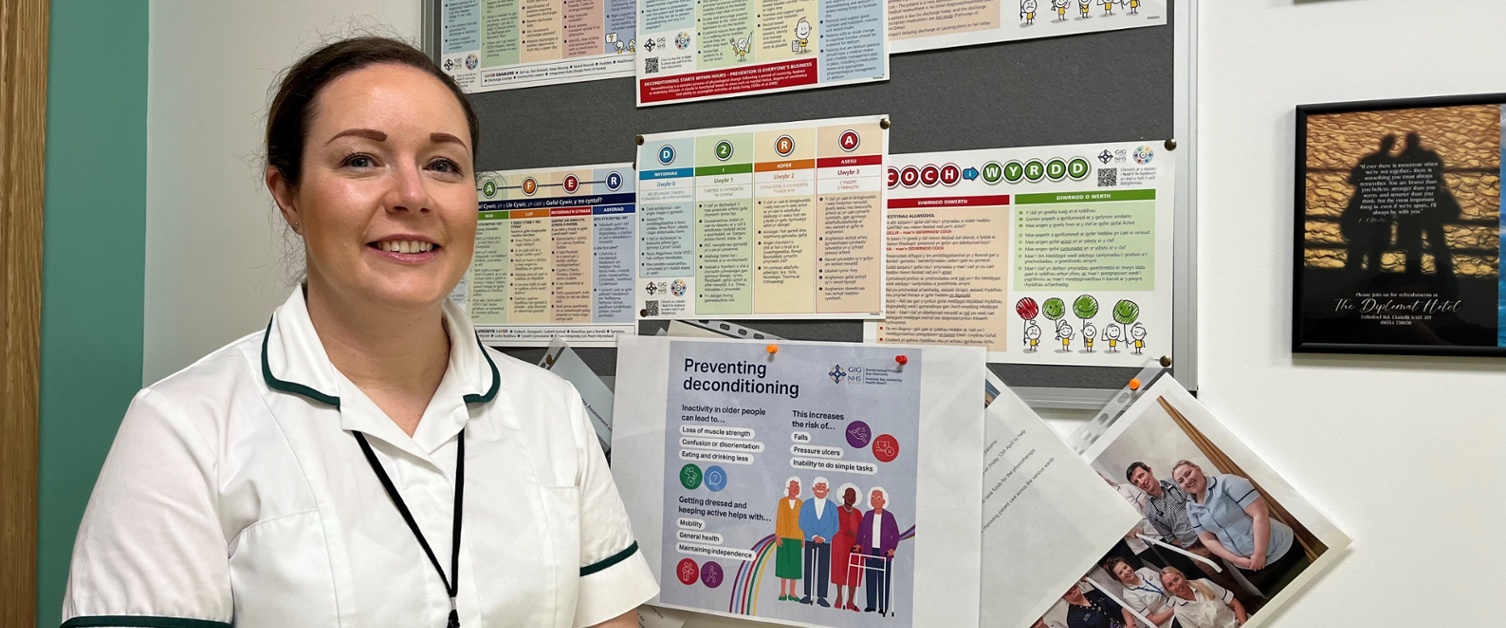
PICTURED: Sarah Morse, Clinical Lead for Occupational Therapy Services in Morriston Hospital’s Unscheduled Emergency Care.
Ensuring patients enjoy the festive period at home – not in hospital – with loved ones is high on our list this Christmas. But we need your help to make this possible.
There’s no place like home when it comes to ensuring patients are in the best place – logistically and physically – to continue their recovery. If your relative has completed their treatment and they’ve been told they can be discharged, please take them home.
Not only does this allow patients to be in familiar surroundings, it also plays a vitally important part in maintaining physical and mental health and reduces the danger of catching infections such as covid, flu and hospital acquired pneumonias.
 Inactivity and inappropriately prolonged bed rest in older people can lead to deconditioning, which is the loss of muscle strength together with mental and functional decline.
Inactivity and inappropriately prolonged bed rest in older people can lead to deconditioning, which is the loss of muscle strength together with mental and functional decline.
Deconditioning can affect anyone, regardless of age, but its impacts are particularly devastating for older and frail individuals.
The stark reality is that 10 days of bed rest can lead to a level of muscle loss equivalent to 10 years of ageing.
PICTURED: Keeping active, when possible, throughout a stay in hospital can reduce deconditioning.
Spending days in hospital can also have an effect on a patient’s mental wellbeing. As some wards don’t have windows or clocks to show whether it’s night or day, this can result in further confusion for patients and impact their recovery.
For patients who do remain in hospital to receive their care, keeping active is important – particularly as patients spend up to 83 per cent of their time in bed.
Sarah Morse is the Clinical Lead for Occupational Therapy Services in Morriston Hospital’s Unscheduled Emergency Care.
Sarah said: “A common misconception is that hospitals are the best place for patients to continue their care.
“While for some patients that may be true, being in familiar surroundings and receiving follow up care at home is the best and safest option for the majority.
“Across our main hospital sites, we have many patients who are clinically well enough to leave but for a number of reasons they can’t go - meaning they stay in hospital days or weeks longer than clinically necessary.
 “That extra time spent in hospital leads to deconditioning, which sets a patient back in their recovery.
“That extra time spent in hospital leads to deconditioning, which sets a patient back in their recovery.
“Patients should be aware that when they come into hospital, they are not here to stay as it’s not the best place to be once they are ready to be discharged clinically.
“Deconditioning is a massive risk to a patient who is in hospital but should be in their own home, or normal place of residency.
PICTURED: (From left) Rebecca Lewis, Occupational Therapist; Sarah Morse, Clinical Lead Occupational Therapist; Daisy Prichard, Occupational Therapist; Dawn Jones, Occupational Therapy Technician; Lisa Davies, Patient Flow Co-ordinator; volunteer Kyaw Tun and Richard Young, Clinical Nurse Specialist for Care of the Elderly.
“Around 47 per cent of patients have their discharge delayed by deconditioning, so it is really important that we do what we can to prevent it.”
Staying hydrated and simple things such as getting dressed in everyday attire can help patients during the time spent in hospital.
Sarah added: “It can be really hard to get into a daily routine when you’re in hospital, but the simple things can make a difference and both staff and patients have to be aware of them. This can include patients going to the toilet independently and eating their meals in the chair and not in bed.
“Ensuring patients are out of bed, dressed in their own clothes and hydrated will help a patient leave hospital as soon as they are able to.
“Some patients will wear their pyjamas all day, but that’s not something they’d do at home. So they are encouraged to wear normal clothes throughout the day.
“Footwear is also a factor. I don’t think people are aware they can wear their own shoes whilst in hospital, which are good in terms of comfort and avoiding falls.
“One in six older patients who normally walk independently need help with walking on discharge from hospital, so this is a hugely important thing to be aware of.”
Rydym yn croesawu gohebiaeth a galwadau ffôn yn y Gymraeg neu'r Saesneg. Atebir gohebiaeth Gymraeg yn y Gymraeg, ac ni fydd hyn yn arwain at oedi. Mae’r dudalen hon ar gael yn Gymraeg drwy bwyso’r botwm ar y dde ar frig y dudalen.
We welcome correspondence and telephone calls in Welsh or English. Welsh language correspondence will be replied to in Welsh, and this will not lead to a delay. This page is available in Welsh by clicking ‘Cymraeg’ at the top right of this page.